Immunotherapy with checkpoint inhibitors
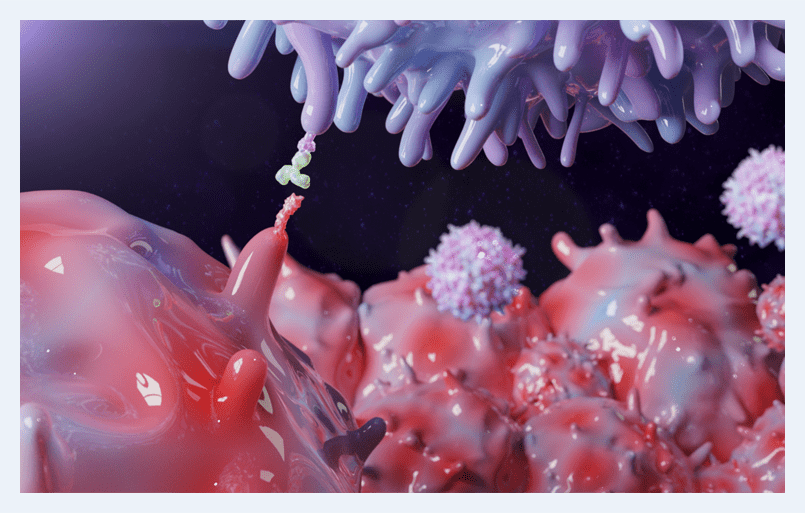
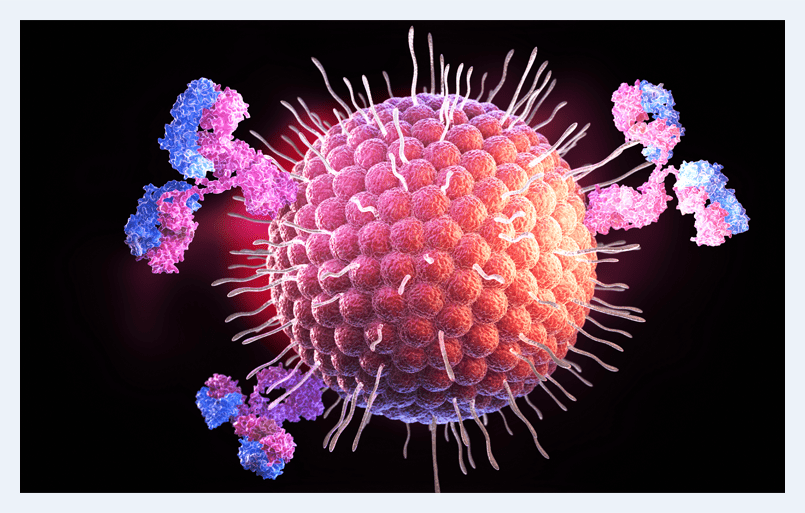
Tumor cells take advantage of the breaks in the immune system. Tumor cells express immune checkpoint molecules to actively turn down the immune response against them. Tumor cells express PD–L1 on their membranes and surfaces. When combined with the PD–1 that are found on the T-lymphocyte cells, there is the resulting down-regulation of immunity. The new checkpoint inhibitors target these receptors and can stop tumor cells from suppressing the T lymphocytes, thus allowing your T lymphocytes to be reactivated in the fight for cancer. We now know that PD–L1 expression by tumor cells is an essential mechanism of tumor immune invasion. CTLA 4 check point inhibitors are also utilized. We are now combining several modes of immunotherapy, which has dramatically shifted the landscape of cancer care and survival.
These new checkpoint inhibitors block pathways and have become a real paradigm shift in the treatment of patients with advanced cancers and are now the standard of care for several cancer types. We are still learning about the optimal dose and timing of radiation and other vaccines that have recently become available. The data from clinical trials of checkpoint therapies are changing the shape of previously known survival curves for cancer patients undergoing treatment.
Checkpoint inhibitors can worsen your cancer and make it more aggressive
One problem does exist with these checkpoint inhibitors. Between 4% and 29% of patients exhibit a hyper progressive or pseudo-progression disease state. In this disease, cancer has accelerated growth. It is correlated with the worst chance of survival. Recent studies have shown that lower dose checkpoint inhibitors may not cause the progression of the disease. If the patient has an elevated microsatellite instability and elevated tumor mutational Burden and/or upregulated PD L1 expression, then they are candidates for checkpoint inhibitors.
Research suggests that the evaluation of circulating cancer cells before and after the administration of checkpoint inhibitors would be a useful tool to ascertain the efficacy of their administration.
Checkpoint inhibitor failures
The reason not all patients respond to checkpoint inhibitors is because of the immune systems tumor microenvironment and immune suppression cells. There is an exhaustion of the T lymphocyte cell. The study suggests that to maximize the body’s immune system's and the therapeutic effect of the checkpoint inhibitors, we need to optimize the T-lymphocyte function. We have now developed new methods of T-cell expansion and augmentation to facilitate checkpoint inhibitor success. It is these tumor-infiltrating lymphocytes that enhance the therapeutic response in human tumors. In this regard, we are using therapies to upregulate T lymphocytes and improve the patient’s underlying immune function.
Recent studies have also shown that THC and marijuana can reduce the effectiveness of this checkpoint inhibitors. Marijuana and THC can reduce the migration of T lymphocytes and may not be appropriate in many patients, especially those with a low lymphocyte count on a peripheral blood smear that is obtaining immunotherapy checkpoint inhibitors. The outcome of efficacy also depends upon the state of health of our microbiome as well as our underlying immune state.

In a 2020 study at the ASCO clinical Immuno oncology symposium, a survey showed that antibiotics exert a profound effect on the composition of the gut microbiome. This study was entitled “Antibiotic exposure worsens survival and colitis in patients with melanoma receiving checkpoint inhibitors.” Antibiotics interfered with the efficacy of the checkpoint inhibitors and caused increased colitis in these patients.
With the increasing use of checkpoint inhibitors and immunotherapy, we are slowly beginning to realize that many factors are relevant to the success of checkpoint inhibitors.
Myeloid suppressor cells and T regulatory cells can also suppress immunity. I employ various modalities before the institution of checkpoint inhibitors to optimize the patient’s immune system and the T-lymphocyte function to make these new therapies effective.
Combination therapy
works best
Using new molecular genomic testing, we can now develop a personalized treatment program for each patient. This includes targeted low-dose chemotherapy, synergistic natural substances, and immunotherapy with checkpoint inhibitors and immunotherapy with an autologous whole cancer vaccine, dendritic cell vaccine, and supportive oligonucleotide’s (SOT).
If you would like further information on checkpoint inhibitors, please contact us at 727-330-3844.
- Personalized Genomic Molecular Profiling
- Low-dose Chemotherapy
- Natural Synergistic Substance
- Immunotherapy w/ Checkpoint inhibitors
- Immunotherapy w/ Autologous Whole Tumor Vaccine
- Dendritic Cell Vaccine
- Supportive Oligonucleotides (SOT)
Testimonials
Contact Us
Have an emergency or need a consultation? Book your visit with us.
Contact Us
-
Contact Us
(727) 330-3844 -
Send Us an Email
Email Us -
Monday to Friday
9:00 AM to 5:00 PM

